How HVAC technologies Help Reduce the Spread of Infection (Part 2of 2)
January 30, 2013
The Center for Health Design (CHD) estimates that as many as 30 percent of hospital infection threats are airborne and numerous cases of MRSA (Methicillin-resistant Staphylococcus aureus) and other types of infections have been traced directly to problems with ductwork, ventilation controls, air exchange ratios and room pressure balance.
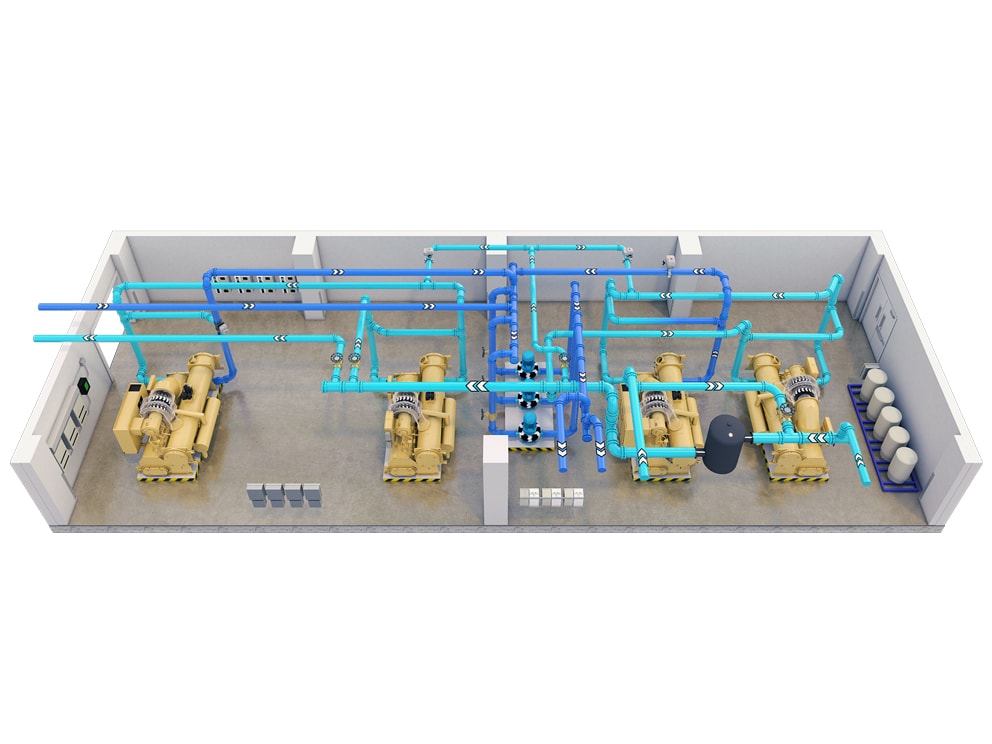
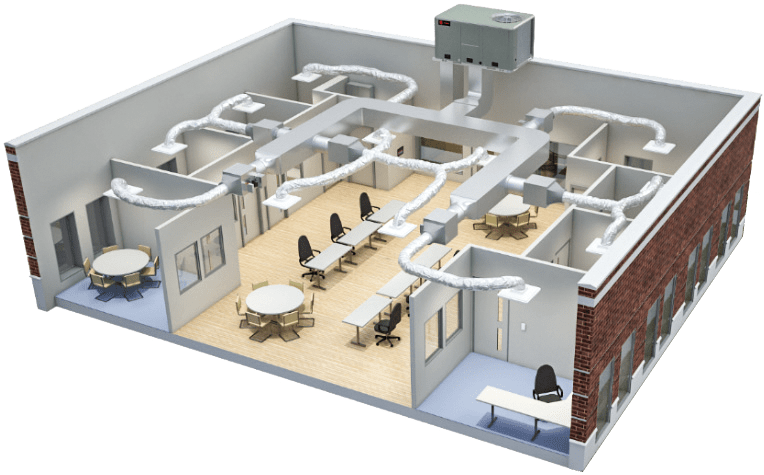
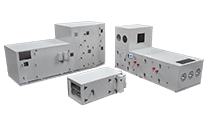
Today’s sophisticated HVAC systems can be configured and controlled to automatically maintain critical performance parameters in multiple hospital units. Advanced building control systems can be programmed to provide the best combination of temperature, relative humidity, room pressure, air exchanges and outdoor air percentage for each hospital unit.
In addition to enhancing comfort and creating the right environment for healing, controlling these and other factors within prescribed parameters for surgical suites, isolation units, patient rooms and other critical areas helps reduce the growth and spread of pathogens within and between medical departments.
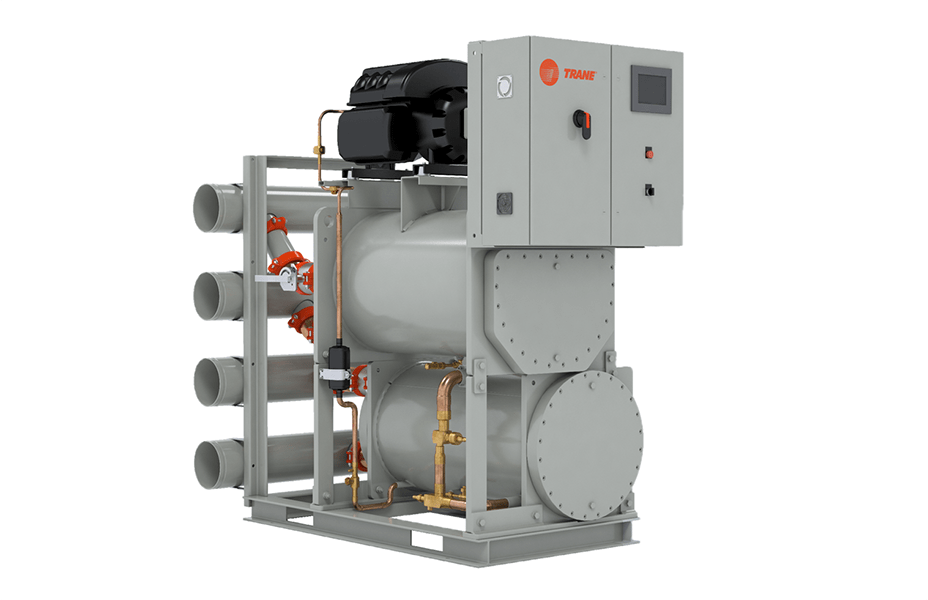
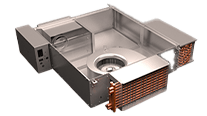
To inhibit the movement of airborne contaminants, ventilation systems must enable frequent air changes with low airflow velocity. Air handlers with low leakage rates meet the high-filtration and static pressure requirements using direct-drive plenum fans and highly efficient fan arrays. A hospital in Michigan credits an 11 percent reduction in hospital-acquired infections to a new ventilation system, along with other changes including expanded use of private rooms and a program to encourage frequent hand washing.
Catalytic air cleaning systems create an extremely effective barrier by combining three technologies. Minimum efficiency reporting value (MERV) 13 filters capture larger particles. Photocatalytic oxidation technologies help eliminate volatile organic compounds, bacteria and other small living organisms. Ultraviolet germicidal irradiation technologies help prevent microorganisms from reproducing.
Creating the best possible physical environment
Maintaining optimum temperature and humidity levels is essential to creating a comfortable indoor environment for patients, physicians, staff members and visitors. But these factors can also have a significant effect on patient outcomes.
For example, standards set by the American Institute of Architects (AIA) Academy of Architecture for Health, U.S. Veterans Healthcare Administration and other healthcare authorities recommend keeping operating room temperatures in the 68-75 degree F range and relative humidity between 30 and 60 percent to create the ideal conditions for the patient and surgical team. Temperatures that are either higher or lower can increase the risk of infection at the surgical site. Higher humidity levels can create the moist conditions that promote the growth and spread of pathogens.
Controlling room pressure also helps prevent the migration of airborne contaminants from one unit to another. For example, isolation rooms need to be kept at a negative pressure so that air flows into the room, helping to keep infection agents from spreading. Conversely, keeping operating rooms at a positive pressure relative to other hospital areas helps prevent the movement of pathogens into surgery suites.
Adding sophisticated sensors to the HVAC system can help healthcare organizations do a better job of monitoring for bacteria, viruses, particulates, pressure and moisture.
Building automation systems can monitor critical areas, automatically correct anomalies and alert the facilities team if problems occur. After simply changing the way it monitors and maintains temperature and relative humidity levels, a Maine hospital reports that it cut the number of hospital-acquired infections in half.
Advanced high performance building technologies and practices and “smart” service and maintenance options enable facilities teams to define HVAC system performance standards and tolerances. These technologies and options also enable facilities teams to maintain optimum performance levels in critical hospital units.
Effective maintenance strategy improves system performance
HVAC and other building systems that are not performing at their original design performance levels can allow indoor air quality to deteriorate and create an environment where pathogens are more likely to grow and spread.
New smart service options make use of advanced technologies and the availability of system performance data to restore and maintain original design performance levels. With a smart service approach, data from building systems and controls is continuously collected, interpreted and acted upon. Hospital facilities teams have the tools to improve building system reliability and uptime, identify and address performance issues before they can cause a system failure, and resolve problems quickly and efficiently.
Regardless of a particular hospital’s approach to building system maintenance, conducting a critical system audit (CSA) is a good starting point to help the organization find and proactively address potential system reliability problems and identify and prioritize energy conservation measures.
Many hospitals choose to work with a third-party energy engineer or energy services company that understands their facility and its impact on their business to conduct an effective CSA. They find that a CSA pays for itself many times over by enabling the organization to reduce energy consumption, save operating costs, support their organization’s goals and improve building system reliability.
Leading healthcare organizations recognize the essential role that a high performance building can play in helping to create the best possible physical environment and achieve their patient-care mission. With HAI one of the greatest threats to positive patient outcomes, hospitals must recognize that creating and maintaining a healthy physical environment is a critical element of any effective infection control initiative.