Improving Physical Environment to Maximize Infection Control (Part 1 of 2)
January 23, 2013
Reducing the incidence of hospital-acquired infection (HAI) is a priority for everyone connected with the healthcare industry. The reasons are obvious. According to the U.S. Department of Health and Human Services, improving HAI rates by 40 percent from a 2010 baseline would save more than 60,000 lives and prevent 1.8 million patient injuries by 2013.
Reducing HAIs would also have an enormous impact on healthcare costs, putting a serious dent in a problem that costs the U.S. healthcare system between $25 billion and $35 billion a year, according to various estimates.
Healthcare professionals recognize that improving hand hygiene, reducing the number of patients in a room, educating staff and visitors, improving waste and laundry management, and creating an effective anti-infection culture are among the best ways to reduce HAIs. But many also recognize building improvements and modifications should be part of a holistic approach to reducing the number of HAIs and improving the physical environment of care.
Healthy buildings help hospitals improve patient care
Ninety-six percent of healthcare executives see a connection between a hospital’s physical environment and positive patient outcomes, according to a survey we conducted at Trane.
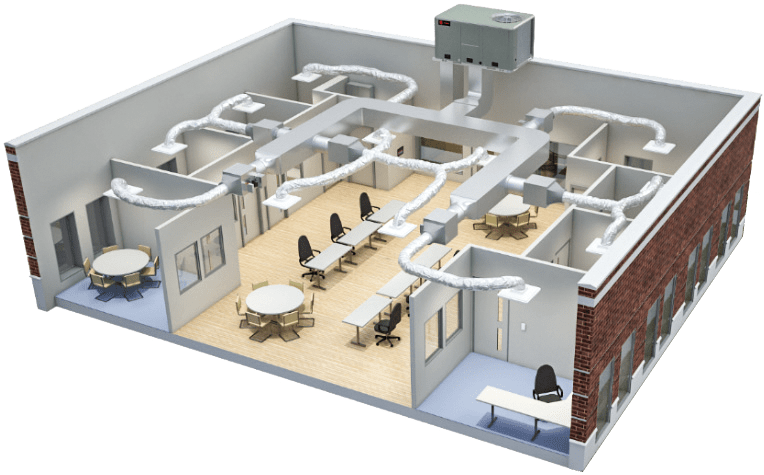
Indoor air quality (IAQ) merits serious attention in any comprehensive infection-control initiative. The Center for Health Design (CHD) conducted research that found 120 independent studies linking IAQ and other physical factors to infection rates. In addition, the World Health Organization includes recommendations for improving IAQ in its Practical Guidelines for Infection Control in Health Care Facilities, and the Joint Commission considers air quality standards in its accreditation process, according to Joint Commission’s published guidelines.
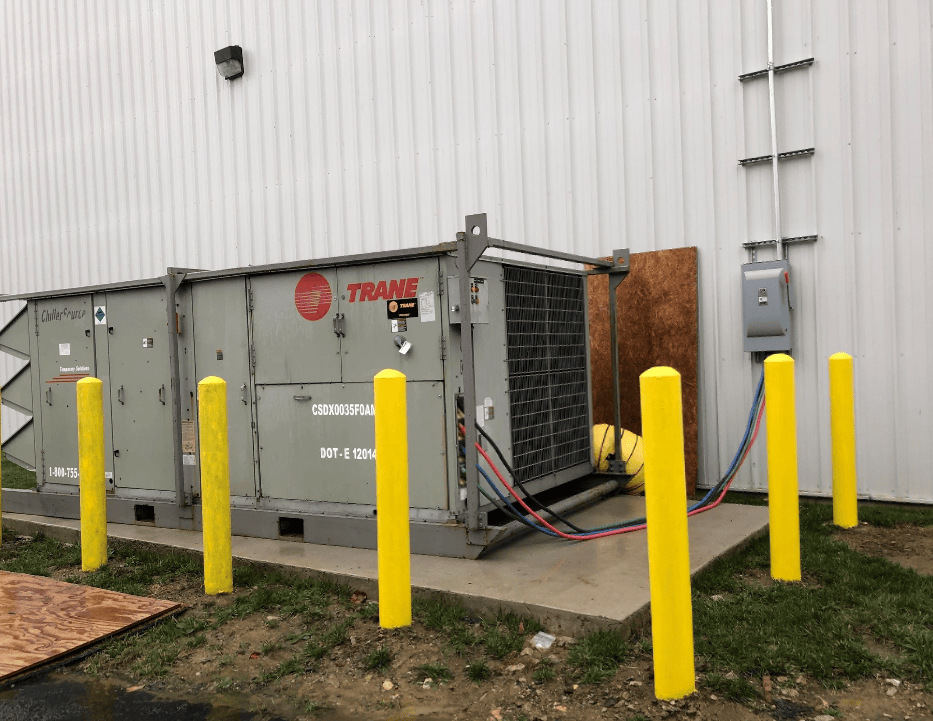
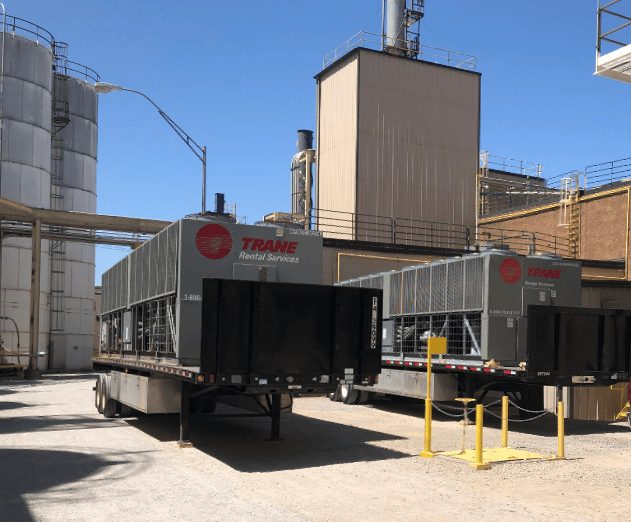
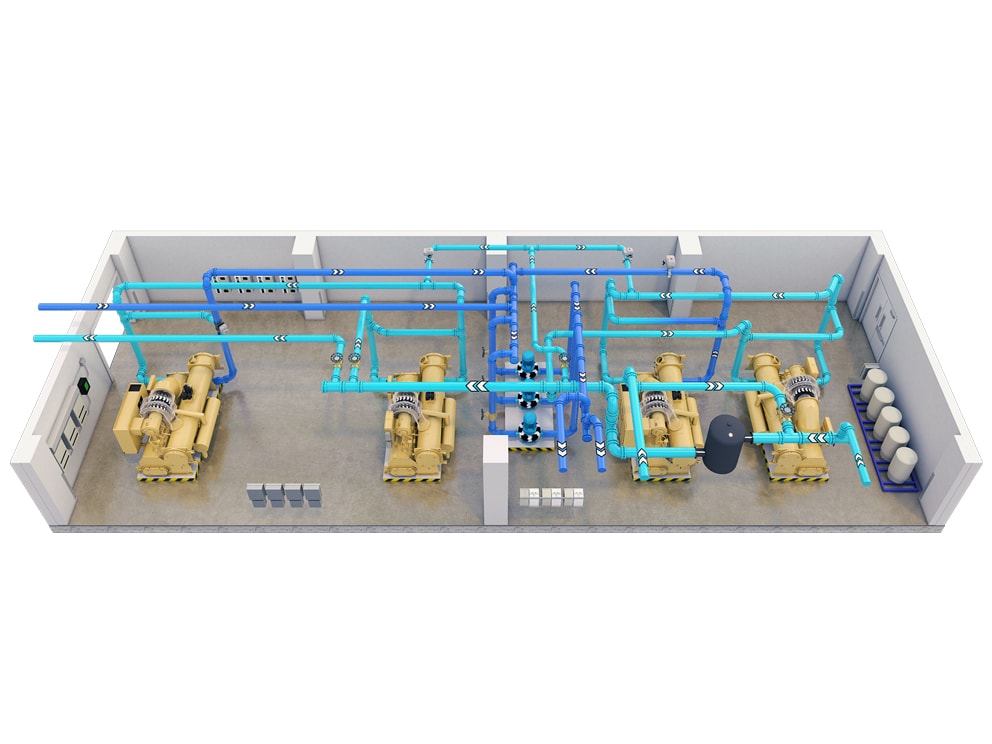
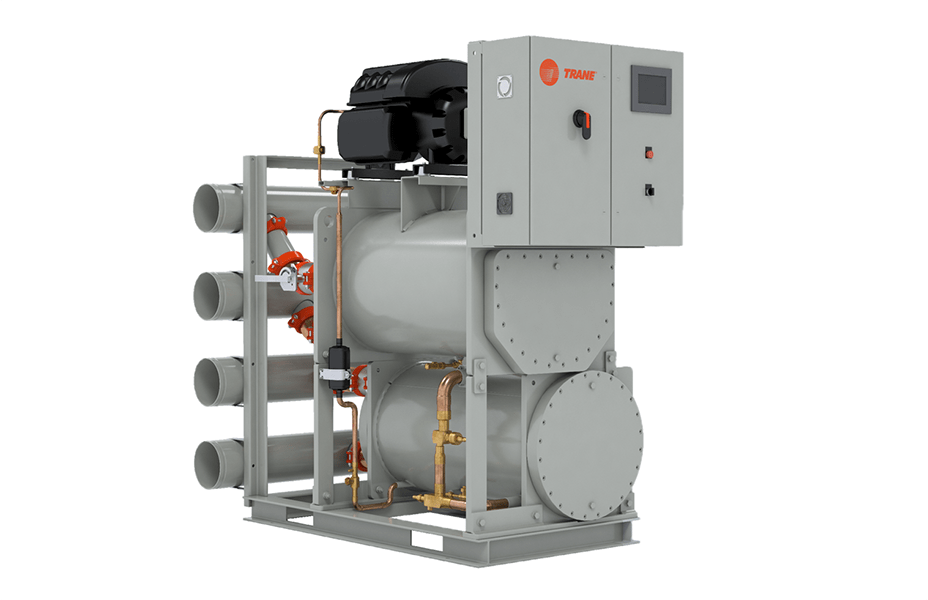
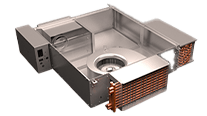
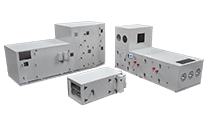
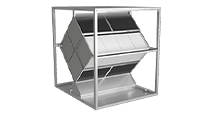
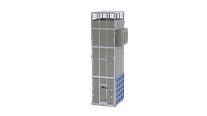
Modern heating, ventilating and air conditioning (HVAC) technologies can help healthcare organizations combat the airborne pathogens that spread infections. New facilities can be equipped with systems that help control pathogens and existing buildings can be retrofit with these technologies.
While economic and political uncertainty are causing many healthcare organizations to reduce or postpone new construction plans, several national surveys show a willingness by hospitals to invest in building improvements and renovations. Much of their planning focuses on efforts to address aging infrastructure problems to improve the quality of patient care, reduce energy consumption and shrink facilities’ environmental footprints, including making strategic improvements to HVAC systems to address long term viability of the healthcare facility.
[Up next: Part 2, How HVAC technologies help reduce the spread of infection]